Salina Surgical Hospital (KS) Improves Pain Management and Decreases Opioid Use

As part of the HQIC program, Salina Surgical Hospital (SSH), a 16-bed hospital located in Salina, KS, identified that Opioid Reduction would be a meaningful project for their group since a large portion of the procedures performed in their facility were Total Joint surgeries. This provided a population of patients to work toward improved opioid use while in the hospital, and also to decrease narcotic use post-operatively. SSH identified areas of improvement based on established best practices. As part of their internal evaluation, SSH determined that they were not within the best practice guidelines for pain management for total joint cases according to the CDC Prescribing Guidelines, Opioid Prescribing Engagement Networks-Prescribing Recommendations, and the Prescription Drug and Opioid Abuse Commission.
Goals/Objectives: The goal for the project was to revise routine pain management protocols for all total joint cases to be in line with best practices as outlined in the above-referenced guidelines, including attempting to reduce overall usage at discharge for patients who had been on a preop narcotic. The evaluation revealed:
- Nerve block (intra-operative) usage was 35%, which is below the goal of 75%
- Tylenol and NSAID (intra-operative) usage in the operating room was at 11%, below the goal of 75%
- Non-opioid pain medication-use post-operatively (Tylenol, Ibuprofen, Toradol) fell below the recommended usage
- Discharge prescriptions for narcotics fell out of the best practice recommendations
PLAN: SSH evaluated established best practices that would be the safest for their patients while continuing to control their pain. Planning activities looked not only at inpatient protocols, but also discharge protocols. There is a large concern from the public about being addicted to pain medication, and a lot of patients do not want to take pain medication. Obviously, the inpatient unit used the most narcotics because the patients stay longer, so this is where planning efforts began. A fundamental component of planning was getting all of the key decision makers together to develop the plan. As part of the initial planning, SSH collected baseline data for current pain control modalities and medications for all Total Hip, Knee and Shoulder Replacements (THR, TKR, and TSR). The timeframe for baseline data collection was from July of 2021 through August of 2021. This data was compiled and areas/opportunities for improvement were identified to better meet established best practice guidelines. SSH identified a Physician Champion to assist in developing a revised pain management protocol for all total joint cases and the project team developed percentage goals based on established guidelines (as previously referenced). Additionally, SSH was unsure if the Orthopedic Office was addressing home pain management, so a plan was developed to engage the ambulatory practice in the project as well.
DO: The primary intervention was to adjust routine pain management protocols to reflect best practices. Those best practice protocols came directly from the tools and resources of the HQIC program. SSH worked with the Physician Champion to evaluate those best practices and identify changes that could be made and worked to decrease not only hospital use, but the number of opioids patients were being discharged on. Those changes included:
- Preoperative and intraoperative increases in the use of IV Tylenol/NSAID
- Intraoperatively, using local anesthetic in the joint (Exparel, Lidocaine)
- Postoperative increase in the use of nerve blocks for total joint cases (adductor canal blocks, spinal block, pericapsular nerve group or PENG block)
- Continue preventative pain management modalities for inpatients, such as ice packs, chronic pain management, same day physical therapy, etc.
- Routine inpatient use of postoperative NSAIDs
- Routine inpatient use of postoperative oral Tylenol
- Routine inpatient PRN use of Oxycodone or Tramadol
SSH also contacted Salina Orthopedics regarding pre-surgical office education on pain management. SSH felt it was important to start communicating with patients about the new protocol before they arrived at the hospital for surgery and worked to enhance preop teaching. It was important for patients to understand that their surgeon was trying new ways to control their pain in an effort to reduce their reliance on narcotics. Ensuring that patients had the right expectations for pain control proved to be a very beneficial part of the project. SSH also increased postop check-ins to see how patients were doing with their prescriptions and were they needing more medication. What they found was that patients who were treated under the revised protocols were very happy and had very good postop pain control.
STUDY: SSH decided to test implementation in a single provider practice first, and so data was collected only for the Physician Champion’s total joint cases with the new pain management protocol in place. The re-measurement period was from February 2022 through March of 2022. The Physician Champion already had several best practices in place (i.e., nerve block, Exparel, etc.) so some of those measures did not change. Upon re-measurement, the following areas of improvement were noted:
- Routine use of NSAIDS (Toradol/Ibuprofen)
- Routine use of Tylenol
- PRN Narcotic use decreased by 64% during hospital stay
- Oxycodone used in lieu of Norco 7.5mg
- Only ONE Home Rx for Oxycodone 5mg #50 given at dismissal
Of note, cases where revised protocols were not used were due to specific contraindications, such as allergies, medication tolerance, etc.
ACT TO HOLD THE GAINS: A formal letter, with the findings and recommendations, was sent to all Orthopedic providers, including the hospital’s physician assistants (PA’s). SSH’s Nursing Manager also visited directly with all Orthopedic providers and PA’s regarding the results and recommendations to initiate the new protocol in their practices. It took several months to coordinate with all providers regarding a firm start date for the new pain protocol. Order sets were built into the electronic health record and education was provided. September 1st of 2022 was the official start date for the implementation and monitoring time frame. The Nursing Manager did have to periodically remind some providers to utilize the new pain protocol. This was not met with 100% success as there was reluctance by some. The expanded re-measurement period included September and October of 2022. The results showed significant improvement for those who used the new protocol in the amounts of opioids used for pain control during the patient’s hospital stay:
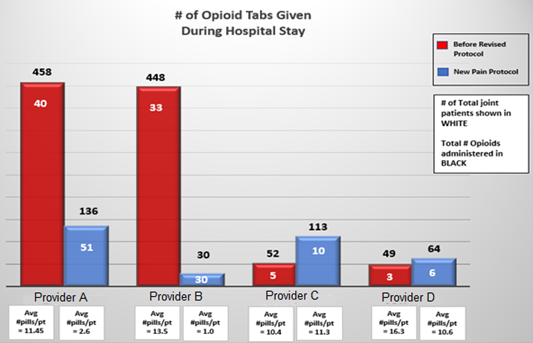
As you can see, for Provider A, despite an increase in the number of surgical patients, the overall number of opioids still decreased significantly from an average of 11.45 pills per patient to 2.6 pills per patient. Decreases in pills per patient were observed for three of the four providers being studied during this period.
Part of the success has included the nurses fully adopting non-pharmacological interventions while the patient is in the hospital, like using ice packs continuously to reduce the swelling, and emphasizing these non-pharmacological options as a key part of the discharge instructions (i.e., postop teaching, exercise, icing)
In December of 2022, the expanded results were sent via letter to all orthopedic providers and PAs showing the significant improvement, and plans were made to discuss the results individually with the providers not using the new protocol consistently to encourage improved use of the protocol.
As part of this broader sharing, the Pharmacist in Charge (PIC) expressed concern about possible GI complications from increased/routine NSAID use and suggested adding proton pump inhibitors for those patients not already taking at home. Routine proton pump inhibitor was added to all total joint order sets. If the patient is on a home proton pump inhibitor, they will resume the medication postoperatively.
Anecdotally, the pharmacy nurses reported noticing a significant reduction in the number of opioids requested by the Inpatient Department since the new protocol was implemented. An unintended consequence of this change is that Oral Opioids are expiring in the pharmacy for the first time. Also, Orthopedic providers have adopted the new pain management protocol for both inpatient and outpatient surgeries and continue to utilize the established best practices when prescribing opioids for home use.
As of April 2023, SSH has seen an overall decrease in the number of opioids administered for these identified case types by 66%, which is consistent with the decrease observed with the individual Physician Champion’s results. SSH’s next steps include ongoing data collection to maintain current gains.